Taken from http://abcplus.net/pain-management/
How Can the Symptoms Be Managed?
Without a cure for FMS, one might wonder if there’s any hope at all for fibromyalgia sufferers. The answer? YES, there is! Though there is not yet a cure, many options are available for successfully treating or managing the symptoms of FMS. The overly goal, though, can be characterized as avoiding your triggers, whether they are symptoms, like sensitivity to touch, or activities, like repetitive lifting, that will flare-up your fibro pain. Here is an overview (more detailed posts are under the section “Treatment Options”):
Medication
There are currently 3 medications that are approved by the United States Food and Drug Administration for treating fibromyalgia pain: Lyrica (pregabalin) in 2007, Cymbalta (duloxetine) in 2008, and Savella (milnacipran) in 2009. Exactly how these medications work in the body is not known (sounds counterintuitive doesn’t it; how can you make something but not know how it works??), but the following are scientists’ most educated guesses on the subject.
Lyrica is an anti-seizure medication that works by blocking signals to the brain, which in the case of FMS are pain signals sent to the brain by overactive nerves in the muscles. Similar to Lyrica is Neurontin (gabapentin), which works in the same way.
Cymbalta and Savella are both antidepressants in the class of serotonin and norepinephrine reuptake inhibitors (SNRIs). Serotonin is a neurotransmitter and hormone that your body produces for use in mood regulation and pain perception and norepinephrine is a neurotransmitter and hormone that impacts your brain’s fight-or-flight response, pain perception, moods and emotions, and cognition. SNRIs work to prevent the reuptake–the re-absorption of secreted neurotransmitters–of serotonin and norepinephrine, thereby increasing their amounts and allowing them to continue helping to improve depression, anxiety, and even the brain’s reception of pain. Similar to Cymbalta and Savella are Elavil (amitriptyline), Flexeril (cyclobenzaprine) (also a muscle relaxant), and Effexor (venlafaxine).
Other drug options are opioid analgesics like Ultram (Tramadol) that can help with pain , dopamine–a neurotransmitter and hormone similar to serotonin and norepinephrine but also affecting cognition, motivation, sleep, and memory– enhancers that can help with pain, and muscle relaxers like Flexeril that ease muscle tension and spasms. Even non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen as well as topical muscle pain relievers like lidocaine, capsaicin, menthol, or camphor (often used to treat pain from arthritis) can also ease FMS pain and pain-increasing symptoms. Sleeping medications like Desyrel (trazodone) or Ambien (zolpidem) and serotonin boosters and alerting medications like Zoloft (sertraline) and Nuvigil (armodafinil) may also be prescribed for help with sleep disorders and difficulties and fatigue.
I currently take the max dose of Lyrica for pain and it has helped a lot with my overall, non-acute pain. I am also trying Pristiq (desvenlafaxine), an SNRI class anti-depressant, to help with fatigue and depression, but it’s not working. My fatigue has actually gotten worse. I’m thinking about asking my doctor for an alerting medication like Nuvigil or Provigil instead. As needed, I will take Flexeril for muscle spasms and muscle pain caused by tension or overworking.
Physical Therapy (aka Physiotherapy) and Exercise
Physical therapy (PT) is mainly the use of manual therapy and exercise to increase mobility, strength, flexibility, endurance, and balance, relieve pain, and reduce joint swelling, especially after an injury. Manual therapies used in physical therapy include manipulation (applying various levels of pressure to the joints with the hands or a specialized device), mobilization (slowly applying measured movements to the bones and joints to move them back where they are supposed to be), and massage (applying various levels of pressure to the soft tissues). Additional techniques used in physical therapy are water therapy, electrical stimulation, the application of heat or cold possibly with water (hydrotherapy), and ultrasound. At-home exercises such as stretching, walking, and core strengthening are usually prescribed by physical therapists to supplement their treatment.
Since FMS is a nerve pain disorder and not an actual “physical” disorder (in the sense that nothing is physically wrong or injured), how can physical therapy and exercise be beneficial to FMS sufferers? Well, physical therapy can improve your muscle flexibility, relax muscle tension, and teach you how to use your muscles more efficiently, thereby minimizing the tension, stiffness, and guarding that result from and further cause FMS pain. Also, as with other chronic pain illnesses such as arthritis, regular movement is known to help with fibromyalgia pain whereas inactivity perpetuates it. These benefits will also help prevent future physical injuries which would trigger more pain.
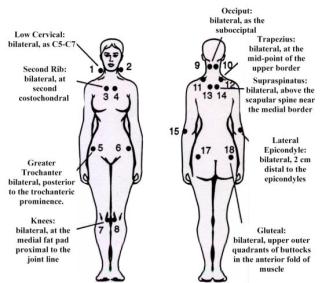
Interestingly, some of our FMS tender points can also be myofascial trigger points (tight, hypersensitive nodules found in the muscle and connective tissue throughout it that are painful and refer pain to other areas) and PT can provide myofascial release and other trigger-point therapies (injections, stretching with heat, and topical medication).
Soon, I’ll be starting physical therapy for the cartilage loss in my right knee and then, hopefully, for my right shoulder, whatever is wrong with it.
Complementary and Alternative Therapies
Complementary therapies are those used in conjunction with conventional medicine–medication, surgery, and some manual therapies–while alternative therapy is used in place of conventional medicine. Complementary and alternative medicine (CAM) can be very beneficial to fibromyalgia sufferers and includes:
- chiropractic therapy–manipulation and adjustment of the body’s musculoskeletal structures, such as the spinal column, to correct structural alignment and relieve nerve pressure and muscle tension;
- osteopathic manipulative treatment (OMT) or osteopathic manipulative medicine (OMM)–a gentler and more ranged form of chiropractic;
- massage therapy, particularly acupressure and deep tissue–manipulation of the body’s soft tissues, muscles, tendons, and ligaments to release tension and pressure as well as reduce stress and anxiety;
- acupuncture–the insertion of very thin needles into the skin and underlying tissues at specific points on the body to increase blood flow and the natural production of the neurotransmitters that decrease pain;
- movement therapies (in other words, exercise)–physical activities such as yoga, tai chi, aerobics (especially water aerobics in a warm pool aka water therapy/hydrotherapy), and dance-based exercises to promote a wide range of physical benefits like increased flexibility, strength, stamina, balance, and circulation and reduced pain and stress; a caution: several of these CAM therapies have religious roots and spiritual overtones so if you are uncomfortable with this, please do more research into the therapy that interests you and the motives and beliefs of the specific practitioners that employ it;
- relaxation techniques–techniques such as breathing exercises, progressive muscle relaxation, guided imagery, biofeedback, and aromatherapy that can help you relax emotionally and physically and reduce and manage stress; and
- improving or adjusting diet, taking nutritional supplements, and taking herbal remedies which can relieve IBS reactions, improve sleep, improve fatigue, and even reduce pain; a caution–nutritional supplements and herbs can have reactions with prescription medications so consult with your doctor and/or pharmacist before adding anything new.
As you know, I currently see a chiropractic (though I think she also used osteopathic techniques) because when certain things like my hip or my vertebrae come out of alignment, I definitely notice resulting increases in pain. She also helps a bit with muscle tightness and knots, but I think a massage therapist might be better for that. Once I start physical therapy and get some of their recommendations, I intend to ease into an exercise regimen. My chiropractic has given me two nutritional supplements: MyoCalm PM to relax my muscles before bedtime, thereby making it easier to get comfortable and go to sleep, and FibroPlex to generally help with fibro pain an symptoms (I think…). Additionally, to help me fall asleep and stay asleep, I take melatonin, valerian, and a homeopathic oral spray with flower essences. This combo certainly aids in falling asleep but for some reason even on the best of nights I wake up at least twice during the night. For fatigue, I’ve tried a ginseng complex but it doesn’t seem to do anything. I also drink Tension Tamer tea for sleep and Fast Lane tea for energy from Celestial Seasonings Teas of the Hain Celestial Group in Colorado. Fast Lane, with 10 mg of caffeine more than a regular cup of coffee, is the only thing I’ve tried that has helped me wake up and get up in the morning (unless my fatigue is flaring up, like it is now). The last things I occasionally use are the topical pain relievers Sombra Warm Therapy (with camphor and menthol), Thera-gesic (with menthol and methyl salicylate), and stick-on heat patches as front line defenses for when I’m starting to have a lot of shoulder, back, or neck pain.
There are so many options available out there, but what works for one person does not always work the same way for someone else, so ALWAYS DO YOUR RESEARCH and consult with your doctor(s) before adding a new therapy to your treatment regimen. And always start slow and ease yourself into it. What treatments work for your fibromyalgia or chronic pain?